- What is Pelvic Organ Prolapse?
- What Causes Pelvic Organ Prolapse?
- How is Pelvic Organ Prolapse Diagnosed?
- Is a Pessary a Good Treatment for Prolapse?
- How do Kegel Exercises Help with Pelvic Organ Prolapse?
- How Does Biofeedback Therapy Work?
- Should I Consider Surgery to Treat Prolapse?
Women with Pelvic Organ Prolapse (POP) might consider non-surgical options for managing a prolapse before they turn to surgery. What is Pelvic Organ Prolapse? It’s when a woman’s pelvic organs push down on her vagina, causing uncomfortable pressure. If you experience a feeling like you are sitting on a ball, an urge to urinate so often it interferes with your daily life, or having to strain in order to empty your bowel, you might have POP.
What is Pelvic Organ Prolapse?
 Pelvic Organ Prolapse happens when a woman’s pelvic organs come down and put pressure on the vagina. Those organs in question could be the bladder, uterus, or rectum. The uterus can also descend into the vaginal canal in some cases. That pressure can cause a variety of symptoms that impact urination, bowel movements, lower back pain, or bleeding in some cases.
Pelvic Organ Prolapse happens when a woman’s pelvic organs come down and put pressure on the vagina. Those organs in question could be the bladder, uterus, or rectum. The uterus can also descend into the vaginal canal in some cases. That pressure can cause a variety of symptoms that impact urination, bowel movements, lower back pain, or bleeding in some cases.
Many patients say they have mild symptoms in the morning, but they get worse throughout the day. If you have POP symptoms, you might feel:
- Like you cannot empty your bladder or bowel completely
- Leaking when you urinate
- A sudden, strong urge to pee
- Constipation or pain during bowel movements
- Pain during intercourse
- Like something is bulging out of your vagina
Some patients who have POP have no noticeable symptoms.
What Causes Pelvic Organ Prolapse?
Healthy and strong muscles, tissue and ligaments normally hold a woman’s uterus in place. It’s important for a woman to try to maintain strength in her abdominal and pelvic muscles as she ages. They can weaken in some women because of pregnancy, difficult labor or delivery, advanced aging and loss of estrogen in a woman’s later years. These factors can cause the uterus, bladder or rectum to press down on the vagina, leading to a pelvic organ prolapse.
How is Pelvic Organ Prolapse Diagnosed?
The best way to determine if you have POP is to attend an office visit with your provider. They can examine you to determine if your pelvic floor muscles are still strong enough to hold your pelvic organs in place. Your provider can also run a series of tests to determine which organs might be out of place, and if you have a prolapse or a different medical condition.
Your provider might order one or more of the following four tests:
- Bladder tests. If you are leaking urine, a condition known as incontinence, your provider may start with a test to determine how well your bladder is working.
- Voiding Cystourethrogram. Your provider may order X-rays of your bladder before and after you pee, to determine if there are problems with your bladder or urethra.
- Ultrasound. Sound waves can create an image of your bladder, uterus and rectum on a screen, so your provider can see if any of those organs are pressing down on the vagina.
MRI. A scan using magnetic waves puts together a three-dimensional image of your pelvic organs and the surrounding muscles. This can help your provider make a diagnosis.
Is a Pessary a Good Treatment for Prolapse?
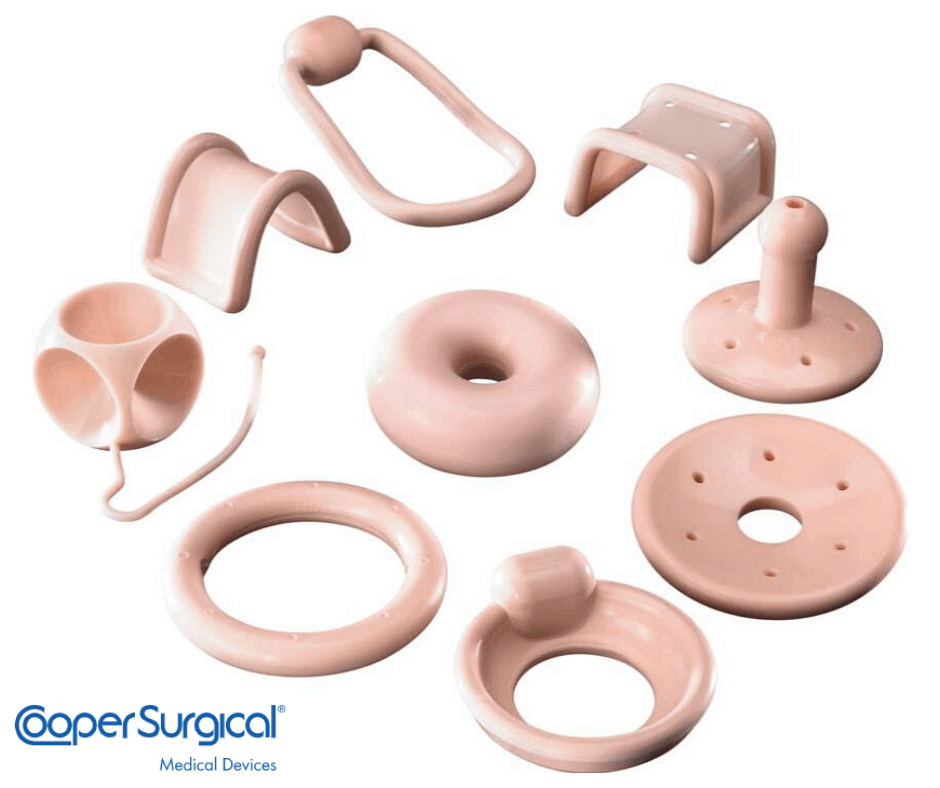 Your provider will consider a few options and might start with a pessary to treat your symptoms. It is one of the most frequently recommended treatments for POP. A pessary is a soft, removable prosthetic device. Most of them are made of medical-grade silicone to be durable. The ring is inserted into the vagina. It holds up your pelvic organs, so they will not put downward pressure on the vagina.
Your provider will consider a few options and might start with a pessary to treat your symptoms. It is one of the most frequently recommended treatments for POP. A pessary is a soft, removable prosthetic device. Most of them are made of medical-grade silicone to be durable. The ring is inserted into the vagina. It holds up your pelvic organs, so they will not put downward pressure on the vagina.
A pessary is a low-cost, minimally invasive treatment. There are two types of pessaries:
- Support Pessary. The support pessary is often the first option recommended by your provider. The most common support pessary is a ring-shaped device, designed to be flexible.
- Space-Filling Pessary. The space-filling pessary is used when a support pessary will not stay in place.
Your provider will need to fit you for a pessary and show you how to insert it. You should plan to have follow-up visits. You will need to clean the device on a regular basis. You can use a pessary temporarily or permanently in some cases.
How do Kegel Exercises Help with Pelvic Organ Prolapse?
Kegel exercises are also called pelvic floor muscle training. The exercises can help strengthen the muscles which hold up your pelvic organs, reducing pressure on the vagina. Your provider can help you set up a routine that matches your needs and your condition.
So which muscles are you trying to exercise? The muscles you use to stop urination in midstream are your pelvic floor muscles. Some providers recommend you start doing Kegel exercises while lying down until you get used to doing them.
The idea is to move your pelvic muscles like you are going to pee, but then suddenly squeeze your muscles to stop the urine from flowing. You tighten and hold the muscles for 5 seconds, then release them for 5 seconds. Set a goal of doing 15 repetitions at a time. Try to do these exercises three times during the course of your day.
Try to focus on only tightening the pelvic floor muscles. Try not to tighten the muscles in your abdomen, thighs or buttocks. Breathe normally while doing Kegel exercises.
Some providers say it can take a few weeks of doing Kegel exercises for them to help improve your condition. You will want to have follow up visits with your provider to monitor your muscle strength.
How Does Biofeedback Therapy Work?
Biofeedback therapy teaches a patient how to contract her pelvic muscles, while using breathing techniques. These are combined with exercises to control the abdominal muscles. Biofeedback therapy helps a patient to relax and reduce stress. A patient learns to consciously decide to slow down her breathing, while tightening pelvic muscles.
Biofeedback therapy could include a few relaxation exercises and techniques:
- Deep breathing
- Tightening and then releasing different muscle groups
- Guided imagery to focus on a specific image to relax your mind
- Mindfulness meditation to release negative emotions
There are some other things you can do to improve POP symptoms. Try to reduce your weight so you do not create additional strain on your pelvic muscles. Eat a high fiber diet to avoid constipation and straining while easing nature. Try not to lift heavy objects, so you do not put pressure on the prolapsed area. Avoid smoking, which can weaken tissues around your pelvic muscles.
Should I Consider Surgery to Treat Prolapse?
Surgery might be an option for you if non-surgical treatments are not working and you have severe symptoms. There are two options:
- Obliterative surgery. This procedure narrows part of the vagina or goes further to close it off. This provides more support to the organs that dropped and put pressure on the vagina. You will no longer be able to have intercourse after this procedure.
- Reconstructive surgery. This procedure tries to repair the pelvic floor and move organs to where they are supposed to be. This surgery can be done with incisions in the vagina or to the abdomen.
Patients who have surgery to treat POP should expect to take a few weeks off from work as they recover. They should not do any strenuous, physical activities for six weeks. A patient’s provider can help her determine which non-surgical treatment might be the best choice to manage a prolapse.
